Patient and Family Engagement Framework

The University of Ottawa Heart Institute (UOHI) has a rich history of patient engagement that has spanned decades. The Ottawa Heart Institute Patient Alumni Inc. was started by Mary Clinckett, the former Head of Physiotherapy at the Heart Institute. She recognized a need for patients to be able to continue to be involved with the Institute, to be kept informed about heart disease, treatment and prevention, and to give them an opportunity to contribute to the work and evolution of the Heart Institute. She retired in 1984 and sent letters to former patients inviting them to join the new organization in 1985. It was established in 1989 with a board of directors and constitution, and since then more than 8,000 former patients and their families have maintained an association with the Heart Institute through the Alumni. The Alumni continue to be active partners on our team sitting on committees, initiating patient and family-centred programs and advising on operational and policy development and quality improvement. This organization is UOHI’s most important resource to ensure meaningful, sustainable patient-centred care. Over the years, UOHI has developed a culture of engagement which has resulted in a strong patient-centred approach to care.
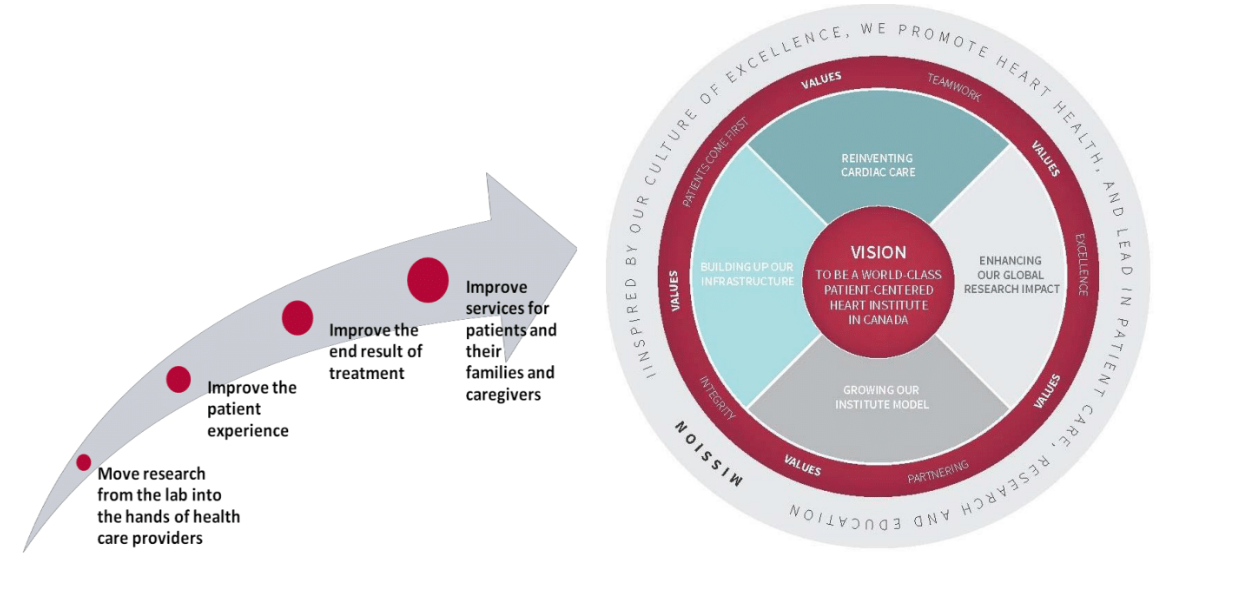
Patient and family-centred care is at the heart of everything we do at the University of Ottawa Heart Institute (UOHI). A key component of this is patient and family engagement and development of a culture of engagement among the hospital leadership, board, researchers, staff, patients and families. Robust patient engagement is a strategic priority for both clinical care and research. We believe this partnership is integral to quality. The values of inclusiveness, support, mutual respect, patient centredness and partnering guide patient and family engagement at UOHI. The construct of patient engagement at UOHI is multi-modal to ensure patient and family engagement across the continuum of their experience: during their care, within the microsystem of the clinic or ward, within the organization and within the larger community. We believe this will improve care at individual, local and system levels. The following are the dimensions of patient engagement at UOHI:
Better Research and Knowledge Translation
Patient and family engagement in research is used to leverage patient experience to improve the quality and relevance of research from a patient perspective. The following principles are integral to this goal:
•Inclusiveness: Patient and family engagement in research integrates diversity of perspectives and research is reflective of that contribution.
•Support: Adequate support and flexibility are provided to patient participants to ensure that they can contribute fully to discussions and decisions.
•Mutual Respect: Researchers, clinicians, patients and families acknowledge and value each other’s expertise and experiential knowledge.
•Patient-Centred: Outcomes relevant to patients such as quality of life are considered and reported along with traditional research outcomes.
•Partnering: Patients and families, researchers and clinicians work together from the beginning to identify problems and gaps, set priorities for research and work together to produce and implement solutions.
Improved Patient Experience
Active patient engagement improves the patient experience. The following principles are integral to this goal:
•Inclusiveness: Factors such as culture, language, accessibility and psychosocial issues will be taken into consideration when developing an individualized plan of care.
•Support: Family, spiritual and staff support are offered and encouraged throughout the continuum of care.
•Patient-Centred: Patients needs, preferences, decisions and personal experience are respected by the team.
•Partnering: Shared decision making is supported by ensuring patients are better informed about choices. A holistic approach to pros and cons of procedures is employed to ensure that the patients are able to make choices that improve their quality of life.
Improved Patient Outcomes
Patient experience is used to help drive better outcomes. The following principles are integral to this goal:
•Inclusiveness: Efforts are put in place to mitigate social determinants of health that may impact care delivery and care transitions. Accessible education and resources are provided to ensure equitable care.
•Support: Patients are supported through transitions to ensure a high standard of care during vulnerable times.
•Patient-Centred: Discussions about what patients value as good outcomes are taken into consideration when developing a care plan and when evaluating and reporting outcomes.
•Partnering: Patients are encouraged to take active ownership and involvement in treatment and self-care. UOHI will provide tools and resources to enable this.
Improved Service Delivery
Co-designing services with patients and families provides better service delivery. The following principles are integral to this goal:
•Inclusiveness: Services are designed to provide equitable care taking into consideration accessibility, social, gender/sex and cultural differences. Effort is taken to integrate diverse perspectives in decision making.
•Support: Support is provided to patients and families to take an active role in providing the patient’s voice in operational/policy decisions that impact service delivery.
•Patient-Centred: Patients values, experiences and perspectives are integrated into service design.
•Partnering: Patients and families are active partners in defining agendas and making operational/policy decisions that impact service delivery.
